INTRODUCTION
Prosthetic devices have been instrumental in transforming the lives of individuals with disabilities, enabling them to regain mobility, independence, and overall quality of life. These artificial limbs and body parts have evolved significantly over the years, integrating cutting-edge technologies to better mimic natural functions ( Park and Shon, 2015). One such technology that has shown immense promise is nanomaterials (NMs), which hold the potential to revolutionize prosthetic devices and further elevate the well-being of disabled individuals. The development of prosthetic devices has a long history, dating back to ancient civilizations. However, with advancements in materials science, engineering, and medical technologies, modern prosthetic devices have become sophisticated tools, enhancing the lives of millions of people worldwide. Prosthetics aim to restore lost or impaired functionality due to amputations, congenital abnormalities, or traumatic injuries. For individuals living with limb loss or disability, prosthetic devices offer numerous physical, psychological, and social benefits. Physically, prosthetic devices enable users to regain mobility, engage in daily activities, and even participate in sports and recreational pursuits. They contribute to improving muscle strength, maintaining bone density, and preventing joint issues caused by disuse. Functionally, prosthetics aid in performing a wide range of tasks, such as walking, grasping objects, writing, and driving, leading to increased independence and reduced dependence on others ( Babizhayev, 2013; Astashina et al., 2014; Jeon et al., 2016; Kaveh et al., 2016; Cellot et al., 2017; Dutta et al., 2017). Psychologically, prosthetic devices play a vital role in restoring body image and self-esteem. By providing a sense of wholeness and normalcy, these devices can alleviate emotional distress caused by limb loss or disability. Socially, prosthetics empower individuals to actively participate in their communities, pursue education, and build fulfilling careers, thus reducing the stigma often associated with disability. Despite the significant progress in prosthetic technology, challenges persist, such as discomfort, limited functionality, and suboptimal integration with the user’s body. Addressing these challenges requires exploring innovative materials and approaches, leading us to the realm of nanomaterials ( Chang et al., 2018; Gade et al., 2018; Pampaloni et al., 2018; Ronzani et al., 2018).
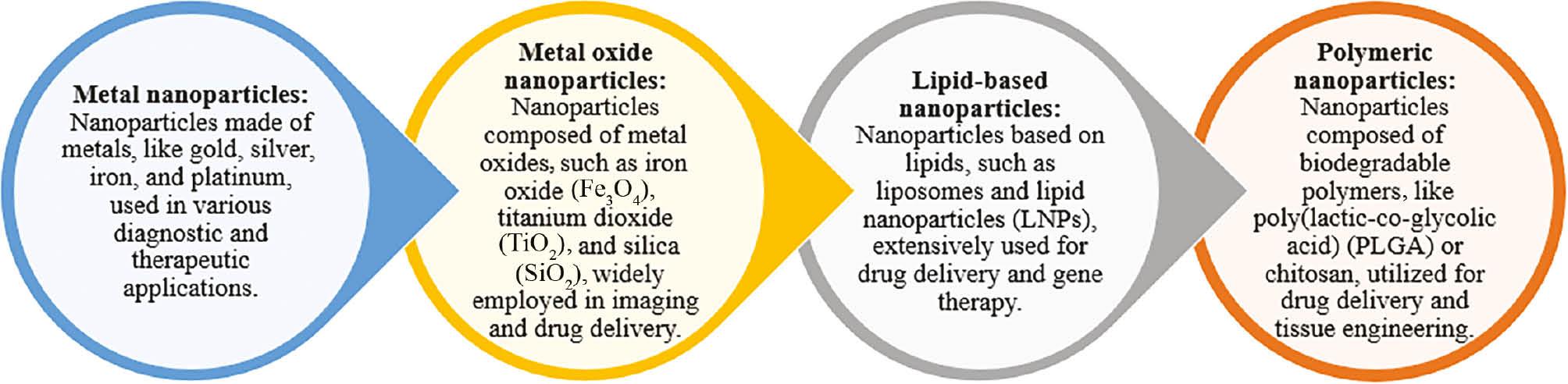
Figure 1 illustrates the classification of nanoparticles used in medical applications. Nanomaterials, as the name suggests, are materials at the nanoscale, typically ranging from 1 to 100 nanometers. At this size, materials exhibit unique properties and behaviors that differ from those of their bulk counterparts. NPs can be engineered to have specific characteristics, such as high surface area, enhanced mechanical strength, and tunable electrical and thermal properties. These attributes make nanomaterials highly attractive for various applications, including those in the medical field ( Kaveh et al., 2016; Cascione et al., 2021). In recent years, researchers and engineers have been exploring the integration of nanomaterials in prosthetic devices to overcome traditional limitations and improve the overall device performance. One of the primary applications of NPs in prosthetics is to enhance the interface between the prosthetic device and the user’s body, optimizing the fit, comfort, and stability. Nanomaterials are being utilized to create advanced socket liners that conform more accurately to the residual limb, reducing pressure points and discomfort. Additionally, NPs can facilitate better attachment methods, ensuring secure and reliable coupling between the prosthetic device and the user. Moreover, nanomaterials offer promising solutions for creating stronger, lighter, and more flexible prosthetic components. Reinforcing structural elements, such as carbon fibers embedded with NPs, result in lightweight yet robust prosthetic limbs. These materials not only improve energy efficiency during movement but also reduce the strain on the user’s intact limbs, minimizing the risk of secondary injuries. Another avenue of exploration involves incorporating nanoscale sensors into prosthetic devices, enabling real-time data collection and feedback ( Chang et al., 2018, 2019; Caviedes et al., 2022; Contreras-Cruz et al., 2023). These sensors can monitor pressure distribution, gait patterns, and even neural signals, allowing for adaptive and intuitive control of the prosthetic limb. Through this literature review, we seek to highlight the immense potential of nanomaterials in prosthetic devices and underscore their crucial role in improving the quality of life for individuals with disabilities. Prosthetic devices have long been instrumental in enhancing the lives of people with disabilities, and advancements in nanomaterials offer promising avenues to further enhance the functionality, comfort, and adaptability of these devices. This literature review aims to shed light on the various applications of nanomaterials in prosthetics and emphasizes the significance of continued research in this interdisciplinary field. By leveraging the unique properties of nanomaterials, we can strive toward developing ideal prosthetic limbs that truly empower individuals with disabilities and provide them with an enhanced quality of life. For literature review, we have extensively sourced research papers from the Scopus database, ensuring a comprehensive and authoritative collection of literature. This methodical approach has enabled us to gather a wide range of pivotal studies, providing a solid foundation for our analysis and conclusions. Our research work employs a systematic literature review design, meticulously analyzing studies sourced primarily from the Scopus database. We focus on the integration of nanotechnology in prosthetic devices, covering a broad spectrum of study designs including randomized controlled trials, observational studies, and qualitative research. The study setting spans global research initiatives, particularly emphasizing advancements in biomedicine and materials science that enhance prosthetic performance and adaptability. Through this comprehensive approach, we aim to encapsulate diverse technological innovations, material engineering breakthroughs, and their clinical applications, reflecting a wide-ranging impact on the development of next-generation prosthetic devices. In our research, we utilized a strategic selection of Medical Subject Headings (MeSH) keywords, including nanotechnology, prostheses and implants, biocompatible materials, biomedical engineering, tissue engineering, nanocomposites, bionics, rehabilitation, sensory feedback, and materials science. These keywords were meticulously combined to refine and target our search for relevant articles, ensuring a comprehensive review of the latest advancements in nanotechnology and prosthetic devices. For our manuscript, we systematically extracted data using a standardized form, capturing author details, study design, setting, participant characteristics, intervention specifics, and key findings. Each article was independently reviewed by two researchers to ensure accuracy and resolve discrepancies through discussion, maintaining a rigorous and consistent data extraction process.
NANOMATERIALS FOR PROSTHETIC DEVICES: HARNESSING UNIQUE PROPERTIES FOR ENHANCED FUNCTIONALITY
The field of prosthetic devices has witnessed significant advancements in recent years, owing to the integration of nanomaterials (NPs) into the design and fabrication of these artificial limbs and body parts. Nanomaterials, with their distinctive properties at the nanoscale, have opened new possibilities for enhancing prosthetic devices’ functionality, comfort, and adaptability. This article explores the key aspects of nanomaterials used in prosthetics, including their unique properties, various types, and the associated advantages and challenges. Nanomaterials are materials engineered at the nanoscale, typically ranging from 1 to 100 nanometers in size. At this scale, materials exhibit novel physical, chemical, and biological properties that differ from those of their bulk counterparts. One of the defining characteristics of nanomaterials is their exceptionally high surface area-to-volume ratio, which leads to increased reactivity and improved mechanical strength. Additionally, quantum effects at the nanoscale give rise to unique optical, electrical, and magnetic behaviors. For prosthetic devices, these unique properties of nanomaterials play a pivotal role in improving the overall performance. For instance, the high surface area of nanoparticles allows for better drug delivery systems and enhanced biocompatibility when incorporated into prosthetic implants ( Babizhayev, 2013). Moreover, the tunable properties of nanomaterials enable the customization of prosthetic devices to cater to individual user needs, promoting a more personalized approach to rehabilitation.
A wide range of nanomaterials have found applications in prosthetic devices. Nanoparticles are particles at the nanoscale that can be engineered from various materials, such as metals, ceramics, and polymers ( Goh et al., 2002; Campbell et al., 2012; Lindberg et al., 2018; Kadhim et al., 2019; Abbas et al., 2020; Abubakre et al., 2023; Siddiqui et al., 2023). These nanoparticles find applications in drug delivery systems, enabling targeted and controlled release of medications to alleviate pain, reduce inflammation, or promote tissue regeneration. In prosthetics, nanoparticles can enhance the biocompatibility of implant materials, leading to improved osseointegration and reduced rejection rates. Nanocomposites are materials composed of a matrix phase reinforced with nanoscale fillers. In prosthetic devices, nanocomposites offer enhanced mechanical properties, such as higher strength, flexibility, and wear resistance. The incorporation of nanofillers, such as carbon nanotubes or graphene, into prosthetic limbs results in lighter yet stronger artificial limbs, reducing the burden on the user and improving their overall mobility. Nanoscale sensors are engineered to detect and measure specific physical or chemical properties at the nanoscale. These sensors can be integrated into prosthetic devices to provide real-time feedback on pressure distribution, temperature, and even neural signals. By monitoring the user’s movements and intentions, nanoscale sensors enable more intuitive and responsive prosthetic control, enhancing user experience and functionality.
Nanomaterials can be engineered to demonstrate exceptional biocompatibility, mitigating the likelihood of adverse reactions and enhancing the successful integration with the biological systems of the host. Nanocomposites and materials reinforced at the nanoscale exhibit superior mechanical properties, including strength, durability, and flexibility, which culminate in the development of prosthetic devices characterized by their lightweight nature and robustness. Moreover, nanoparticles facilitate precise drug delivery mechanisms, enabling localized treatment modalities for pain management and tissue regeneration. Nanomaterials allow for the modification of surface properties, promoting cell adhesion and tissue growth around prosthetic implants. Nanoscale sensors provide real-time data, enabling adaptive and responsive control of prosthetic devices. While nanomaterials offer improved biocompatibility, potential long-term effects and toxicity require careful consideration and thorough testing. The fabrication and integration of nanomaterials into prosthetic devices may pose challenges in terms of scalability and cost-effectiveness. The use of nanomaterials in medical devices may require specific regulatory approvals to ensure safety and efficacy. Some nanomaterials may exhibit altered properties over time, necessitating research into their long-term stability and performance. The integration of nanoscale sensors for neural interface raises ethical concerns regarding privacy, security, and informed consent. Nanomaterials have emerged as a transformative force in the field of prosthetic devices, unlocking new possibilities for enhanced functionality and improved quality of life for individuals with disabilities. Their unique properties, including improved biocompatibility, mechanical strength, and drug delivery capabilities, offer significant advantages in the design and manufacturing of prosthetics ( Wang et al., 2019; Alavi et al., 2022). While challenges such as biocompatibility concerns and manufacturing complexities exist, ongoing research and collaboration between scientists, engineers, and medical professionals hold the key to harnessing the full potential of nanomaterials for prosthetic devices. The continued exploration and integration of nanotechnology in prosthetics promise a future where artificial limbs and body parts can closely mimic natural functions, empowering individuals with disabilities to lead fulfilling and active lives.
NANOMATERIALS IN BONE PROSTHETICS
The incorporation of nanomaterials in bone prosthetics has garnered significant attention from researchers and scientists seeking to improve the performance and biocompatibility of these implants. Numerous studies have investigated the potential of nanomaterials, such as nanoparticles and nanocomposites, in enhancing bone prosthetics’ osseointegration and overall functionality ( Bulusu et al., 2017; Velu et al., 2020). Research has focused on understanding the interactions between nanomaterials and bone tissue, evaluating the mechanical properties of nanocomposite implants, and investigating the controlled release of therapeutic agents from nanoparticle-based coatings. Moreover, studies have explored the impact of nanotopography on cell adhesion and proliferation, as well as the modulation of the inflammatory response at the implant site. Collectively, the body of research highlights the promise of nanomaterials in revolutionizing bone prosthetics and laying the groundwork for more efficient and patient-specific solutions. The introduction of nanomaterials has significantly improved the performance and durability of bone prostheses, addressing some of the limitations of conventional materials. One key aspect is the enhanced mechanical strength of nanocomposites, which exhibit superior load-bearing capacities, reducing the risk of implant failure. Nanocomposite materials, such as carbon nanotube-reinforced polymers, offer a balanced combination of strength and flexibility, leading to implants that more closely mimic natural bone behavior. Additionally, nanomaterials’ high surface area allows for better functionalization, enabling the controlled release of therapeutic agents like antibiotics or growth factors to promote bone regeneration and prevent infections. Furthermore, nanomaterials’ tailored surface properties facilitate improved cell adhesion and integration with the surrounding bone tissue, ensuring better osseointegration and long-term stability. By harnessing the unique properties of nanomaterials, bone prostheses can achieve higher performance levels, reduced wear and tear, and improved longevity, ultimately benefiting patients with enhanced functional outcomes and a better quality of life. Integrating nanomaterials in bone prosthetic devices offers several significant benefits, but it also comes with certain limitations that need to be carefully evaluated. One of the key advantages is the improved biocompatibility of nanomaterials, which can reduce the risk of rejection and inflammation compared to traditional materials. Additionally, nanocomposites’ enhanced mechanical properties contribute to better load distribution and reduced stress shielding, which can promote more natural bone remodeling and reduce the risk of implant loosening. Moreover, nanomaterials’ ability to release therapeutic agents allows for localized and targeted treatment, addressing infection and facilitating bone healing.
However, some limitations must be considered. The long-term effects of nanomaterials on the human body need further investigation, as potential toxicity and accumulation of nanoparticles may raise safety concerns. Furthermore, the cost of producing nanomaterials and their integration into bone prostheses can be higher than conventional materials, potentially impacting affordability and accessibility for patients. Manufacturing complex nanocomposite structures with consistent quality may also present challenges. Additionally, ensuring regulatory compliance and addressing ethical concerns related to using nanomaterials in medical devices are essential aspects that require careful attention. In conclusion, the research on nanomaterials in bone prosthetics reveals a promising path toward more effective and durable implants. The unique properties of nanomaterials, including improved mechanical strength, tailored surface properties, and controlled drug release, offer substantial advantages in enhancing bone prostheses’ functionality and biocompatibility. However, a thorough evaluation of their long-term safety, manufacturing scalability, and cost-effectiveness is crucial to successfully translate these advancements into practical and accessible medical solutions. Overall, nanomaterials hold the potential to revolutionize bone prosthetics and significantly improve the quality of life for individuals with bone-related disabilities and injuries.
NANOMATERIALS IN SKIN PROSTHETICS
Nanomaterials have emerged as innovative solutions in the field of skin prosthetics and wound healing, offering tremendous potential to enhance comfort, functionality, and overall patient outcomes. In skin prosthetics, nanomaterials are utilized to fabricate advanced socket liners, dressings, and cosmetic covers, tailored to provide a more precise fit and improved biomechanical interface between the prosthetic and the residual limb. The incorporation of nanofibers, nanoparticles, and nanocomposites in socket liners enhances their flexibility, breathability, and moisture-wicking properties, reducing friction and discomfort while promoting air circulation, essential for amputees’ skin health ( Reinschmidt et al., 1997; Lu and O’Connor, 1999; Alexander and Andriacchi, 2001). Additionally, nanomaterials enable the development of smart prosthetic coverings with self-healing properties, protecting the underlying components from wear and tear. In wound healing, nanomaterials have been employed to engineer bioactive dressings and scaffolds, facilitating tissue regeneration, and accelerating the healing process. Nanoscale drug delivery systems allow for the controlled release of growth factors and antimicrobial agents directly to the wound site, promoting cell proliferation and reducing the risk of infection. Moreover, nanomaterial-based skin substitutes with tunable mechanical properties have shown promising results in promoting dermal tissue regeneration, offering a viable alternative for patients with extensive skin loss ( Taylor et al., 2005; Ryu et al., 2009).
Comfort and functionality of skin prosthetic devices
Integrating nanomaterials has significantly contributed to enhancing the comfort and functionality of skin prosthetic devices, addressing conventional challenges amputees face. The use of nanofibers and nanocomposites in socket liners provides a lightweight and adaptive fit, conforming precisely to the residual limb’s contours, thus minimizing pressure points and discomfort. These nanomaterials exhibit improved breathability and moisture management, preventing skin irritation and perspiration accumulation, which can lead to infections or skin breakdown. Furthermore, nanomaterials enable the development of multifunctional prosthetic covers, incorporating antimicrobial agents and temperature-regulating properties to enhance hygiene and thermal comfort. In smart prosthetic coverings, self-healing nanomaterials protect the prosthetic components, extending the device’s lifespan and reducing the need for frequent replacements ( Andersen et al., 2010; Cockcroft et al., 2016). Introducing nanomaterial-based bioactive dressings in wound healing also ensures better wound management, promoting an optimal environment for tissue regeneration while providing pain relief and reducing dressing changes, ultimately improving the patient’s comfort and quality of life.
Advantages and potential risks
The application of nanomaterials in skin prosthetics offers numerous advantages, but it is crucial to evaluate potential risks to ensure patient safety and device efficacy. Advantages include improved biocompatibility of nanomaterials, reducing the risk of adverse reactions and infections, which is particularly beneficial for patients with sensitive or compromised skin. The customizability of nanomaterials allows for patient-specific designs, ensuring a more tailored fit and enhanced prosthetic comfort. Furthermore, the enhanced mechanical properties of nanocomposites in socket liners contribute to prosthetic longevity and wear resistance. Nanomaterial-based wound dressings facilitate accelerated healing and reduced scarring, promoting optimal tissue regeneration and recovery. However, potential risks related to nanomaterials must be carefully considered, including concerns about long-term biocompatibility and systemic effects. Certain nanoparticles’ potential toxicity and accumulation in tissues raise questions about their safety over extended periods ( Zotov et al., 2020). Moreover, the manufacturing complexity and cost of nanomaterials may impact the accessibility of advanced skin prosthetics for some patients. Rigorous testing and regulatory oversight are essential to address these concerns and ensure the responsible integration of nanomaterials in skin prosthetics and wound healing applications, maximizing their benefits while minimizing potential patient risks.
NANOMATERIALS IN NERVE PROSTHETICS
Nanomaterial advancements have opened new frontiers in nerve prosthetics and neural interfaces, aiming to restore sensory and motor functions for individuals with neurological impairments. Nanomaterial-based neural interfaces have revolutionized the field of brain–computer interfaces (BCIs) and neural implants, enabling direct communication between the nervous system and external devices ( Yoo et al., 2016; Bahmani Jalali et al., 2018; Liang et al., 2022). Nanomaterials offer unique properties, such as high surface area and tunable electrical conductivity, making them ideal candidates for promoting seamless neural integration. In nerve prosthetics, nanomaterials have played a crucial role in enhancing the biocompatibility and electrochemical properties of neural electrodes, facilitating the long-term stability and reliability of the implant. Moreover, developing nanoscale sensors and actuators has enabled real-time monitoring of neural signals and precise control of prosthetic devices, leading to more natural and intuitive movement. As research in this area continues to evolve, nanomaterial-based nerve prosthetics hold great promise in advancing the field of neural rehabilitation and improving the quality of life for individuals with neurological conditions.
Nanomaterials offer several key advantages in enhancing the interface between prosthetic devices and nerves, facilitating seamless communication and interaction. The high surface area-to-volume ratio of nanomaterials allows for a larger number of neural interfaces in a smaller footprint, enabling higher-resolution recordings and more precise stimulation. Moreover, nanomaterials’ tunable electrical properties enable tailored modulation of neural signals, optimizing the compatibility and specificity of the interface with neural tissue. Nanomaterial-based coatings on neural electrodes promote better biocompatibility and reduce foreign body response, improving long-term stability and minimizing tissue damage. Furthermore, the miniaturization of nanoscale sensors and actuators allows for creating implantable devices that can respond in real time to neural signals, enabling more natural and intuitive control of prosthetic limbs. Nanomaterials’ use in neural interfaces can revolutionize neuroprosthetics, bringing us closer to realizing fully functional and integrated neural rehabilitation technologies.
Integrating nanomaterials in nerve prosthetics not only offers exciting potential benefits but also presents unique challenges that warrant careful consideration. The advantages include improved biocompatibility, which reduces the risk of inflammation and rejection, ensuring the long-term stability of neural interfaces. Nanomaterial-based neural electrodes exhibit enhanced charge transfer capabilities, enabling more efficient and targeted stimulation of neural tissue. Nanoscale sensors and actuators also enable real-time feedback and control, facilitating adaptive and intuitive prosthetic devices. The versatility of nanomaterials allows for their incorporation into various neural interfaces, such as intracortical implants, peripheral nerve interfaces, and neuromuscular interfaces, expanding the scope and applicability of neural rehabilitation technologies. However, challenges include potential long-term biocompatibility concerns, as nanomaterials’ interactions with neural tissue over extended periods are still under investigation. Fabricating nanomaterial-based neural interfaces with consistent quality and scalability remains challenging. Ethical considerations surrounding the use of invasive BCIs and data privacy need careful attention. Additionally, regulatory approval and safety assessments are paramount to ensure responsible translation from the laboratory to clinical applications. Despite these challenges, nanomaterial-based nerve prosthetics hold immense promise in revolutionizing the field of neurorehabilitation, offering groundbreaking possibilities in restoring neural functions and improving the quality of life for individuals with neurological conditions.
NANOMATERIALS IN ELECTRIC AND MYOELECTRIC PROSTHETIC LIMBS
Integrating nanomaterials in electric and myoelectric prosthetic limbs has emerged as a transformative approach, significantly enhancing the functionality, adaptability, and overall performance of these advanced prosthetics. Nanomaterials, such as nanoparticles and nanocomposites, have enabled unprecedented improvements in the design and manufacturing of electric and myoelectric prosthetic limbs, addressing conventional limitations and ushering in a new era of enhanced user experience ( Contreras-Cruz et al., 2023). Nanoparticles are used to optimize the conductive properties of electrode materials, allowing for more precise and efficient signal transmission between nerves and prosthetic components. This results in seamless and intuitive prosthetic limb control based on the user’s intent. Additionally, nanocomposites provide lightweight yet durable structural components, leading to more efficient energy consumption and reduced fatigue for the user. Furthermore, nanomaterial-based sensors enable real-time feedback and adaptability, allowing the prosthetic limb to respond dynamically to changes in the user’s movements and environment. The diverse applications of nanomaterials in electric and myoelectric prosthetic limbs have paved the way for personalized and sophisticated devices that closely mimic natural limb functionality, ultimately empowering individuals with disabilities to lead more independent and fulfilling lives ( Bruni et al., 2023; Kannenberg et al., 2023).
Incorporating nanomaterials has revolutionized the functionality and adaptability of electric and myoelectric prosthetic limbs, overcoming inherent challenges in traditional designs. Nanoparticles are pivotal in improving electrode materials, allowing for more sensitive and accurate sensing of electrical signals from the user’s residual muscles. This enhancement translates into smoother and more precise prosthetic limb control, enabling fine motor movements and intricate tasks that were previously difficult to achieve. Moreover, nanocomposite materials with superior mechanical properties offer a perfect balance of strength and flexibility, resulting in lighter prosthetic limbs that reduce the burden on the user and provide a more comfortable fit. The adaptability of nanomaterials lies in their capacity to integrate sensors that can detect changes in pressure, temperature, and other environmental factors, allowing the prosthetic limb to respond dynamically to different situations. Furthermore, nanoscale actuators and shape memory alloys enable prosthetic devices to adjust their configuration based on the user’s activities, promoting seamless transitions between different modes of operation. As a result, electric and myoelectric prosthetic limbs with embedded nanomaterials have unlocked a new realm of functionality and adaptability, empowering users with enhanced control and responsiveness that mimic the intricacies of natural limb movement ( Chuang et al., 2012; Nowak et al., 2023; Touillet et al., 2023; Vujaklija et al., 2023).
Clinical testing and real-world performance of electric and myoelectric prosthetic limbs with embedded nanomaterials have demonstrated remarkable advancements, validating the promise of nanotechnology in the field of prosthetics. Clinical trials have shown that nanomaterial-based electrodes result in more reliable and robust signal acquisition, improving prosthetic control and reducing signal noise. Users have reported enhanced precision and reduced learning curve with nanomaterial-enhanced prosthetics, making daily activities and task execution smoother and more natural. The lightweight and durable nature of nanocomposite materials has been validated in long-term usage, leading to fewer instances of component wear and damage and ultimately extending the prosthetic limb’s lifespan. Additionally, integrating nanoscale sensors and actuators has enabled prosthetic devices to adapt to dynamic environments, providing users with increased confidence and stability during various activities. However, continuous clinical monitoring and real-world studies are essential to assess nanomaterials’ long-term biocompatibility and safety in contact with human tissues. Furthermore, scalability and cost-effectiveness remain important factors to address, ensuring wider accessibility and affordability of nanomaterial-based prosthetics. Overall, the clinical testing and real-world performance of electric and myoelectric prosthetic limbs with embedded nanomaterials showcase the remarkable advancements made in the field, underscoring the potential of nanotechnology to revolutionize the future of prosthetic technology and significantly improve the quality of life for individuals with limb loss or disability ( Kannenberg et al., 2023).
NANOMATERIALS IN ADAPTIVE DEVICES AND ITEMS FOR DISABLED INDIVIDUALS
Nanomaterials have sparked a wave of innovation in the development of adaptive items and assistive devices, revolutionizing the landscape of accessibility and empowerment for people with disabilities. These advanced materials offer unique properties that enable tailored solutions to address specific needs and challenges faced by individuals with different disabilities. In the realm of adaptive items, nanomaterials are integrated into orthotic and prosthetic devices to improve fit, comfort, and functionality. For instance, carbon nanotubes and nanocomposites are used to create lightweight and flexible orthoses, ensuring optimal support and mobility for individuals with musculoskeletal conditions. In assistive devices, nanoscale sensors and actuators play a pivotal role in creating smart devices that respond to users’ movements and environmental cues. From smart canes with obstacle detection to wearable exoskeletons with real-time feedback, nanomaterials enable seamless integration of technology and human–machine interaction. Moreover, nanomaterial-based coatings enhance the grip and durability of assistive devices, such as adaptive utensils and tools, promoting independence in daily activities. The versatility and customizability of nanomaterials empower designers and engineers to create adaptive items that cater to individual needs, fostering a more inclusive and accessible world for people with disabilities ( Frias et al., 2022; Jung et al., 2022; Sharan et al., 2023).
The potential impact of nanomaterials on various adaptive items is far-reaching, transcending multiple domains and enhancing user experiences in numerous ways. Nanomaterials offer lightweight yet strong reinforcements in sports, resulting in high-performance gear with improved flexibility and durability. Nanocomposite materials used in sports prostheses provide athletes with limb loss or limb difference an opportunity to excel, as these prostheses enable fluid movement and biomechanical efficiency. In clothing and footwear, nanomaterials enhance breathability, moisture-wicking properties, and thermal regulation, ensuring greater comfort and reducing the risk of skin irritations for individuals with sensory sensitivities. Integrating nanoscale sensors in adaptive toys facilitates interactive play experiences, promoting cognitive development and social interaction for children with disabilities. Furthermore, nanomaterial-based adaptive utensils and kitchenware offer ergonomic designs and antimicrobial properties, making meal preparation and dining more accessible and hygienic for individuals with motor impairments. The potential impact of nanomaterials extends beyond the individual user, as advancements in these adaptive items contribute to breaking down societal barriers and stigmas associated with disabilities, fostering a more inclusive and accepting environment. Using nanomaterials in adaptive devices not only brings about practical benefits, but also poses certain challenges that necessitate careful consideration. The lightweight nature of nanocomposite materials in sports items and prostheses reduces user fatigue and improves overall performance. Incorporating nanoscale sensors and actuators in adaptive devices enhances functionality, enabling real-time feedback and adaptive control. Nanomaterial-based coatings offer wear resistance and durability, extending the lifespan of adaptive items. However, challenges lie in ensuring consistent manufacturing and quality control, as the production of nanomaterials and their integration into adaptive devices can be complex and costly. Safety and regulatory considerations must also be addressed, particularly concerning nanoparticles’ potential release and long-term effects on human health. Additionally, accessibility and affordability of nanomaterial-based adaptive devices remain crucial aspects to ensure equitable access for all individuals with disabilities. Ethical considerations related to data privacy and user consent in smart adaptive devices warrant careful attention. Addressing these challenges requires collaboration between researchers, manufacturers, policymakers, and end-users to balance innovation, safety, and accessibility. Despite these challenges, the practical benefits of nanomaterials in adaptive devices have already demonstrated their transformative potential in enhancing the lives of individuals with disabilities, and continued research and innovation in this area hold the key to furthering inclusivity and empowerment for all ( Zhang et al., 2022; Mahjoubi et al., 2023).
HYBRID NANOMATERIALS FOR IDEAL PROSTHETIC LIMBS
The emergence of hybrid nanomaterials marks a significant leap in the quest for optimal prosthetic limb performance. These innovative materials, combining the principles of biomedicine and materials science, are engineered to address the multifaceted challenges of prosthetic devices. Hybrid nanomaterials leverage the synergistic properties of various nanoscale components, such as nanoparticles, nanofibers, and nanocomposites, to create novel prosthetic designs that closely mimic natural limb behavior. By tailoring the material composition at the nanoscale, researchers can achieve a delicate balance of strength, flexibility, and biocompatibility, crucial for successful osseointegration and prolonged use. Moreover, incorporating nanoscale sensors and actuators enables prosthetic limbs to adapt to users’ movements and intentions, leading to more intuitive and responsive control. The exploration of emerging hybrid nanomaterials has the potential to revolutionize the prosthetic industry, paving the way for advanced limb replacements that significantly improve the quality of life for individuals with limb loss or limb impairment ( Hyder et al., 2022; Liaquat et al., 2022; Xing, 2022).
The convergence of biomedicine and materials science has been instrumental in developing advanced nanocomposites, revolutionizing the landscape of prosthetic devices. Biomedicine contributes vital insights into the biological interactions between nanomaterials and living tissues, enabling the design of biocompatible coatings and implants that reduce adverse reactions and promote tissue integration. On the other hand, materials science leverages nanotechnology to engineer nanoscale reinforcements, such as carbon nanotubes, graphene, and bioactive nanoparticles, that enhance the mechanical properties and functionalities of prosthetic components. By tailoring nanocomposites’ surface chemistry and topography, researchers can stimulate cell adhesion and tissue regeneration, essential for successful prosthetic osseointegration. Furthermore, combining biomedicine and materials science enables the controlled release of therapeutic agents from nanomaterials, promoting targeted drug delivery for pain management and tissue healing. This interdisciplinary approach unleashes the full potential of nanocomposites in prosthetic devices, creating more efficient, durable, and user-centric solutions that closely mimic natural limb behavior and function. The incorporation of hybrid nanomaterials in prosthetic devices offers numerous potential advantages and opens up exciting future prospects in the field of prosthetics. First, the tailored properties of hybrid nanocomposites, including improved strength, flexibility, and biocompatibility, enhance prosthetic limb performance and longevity, reducing the need for frequent replacements and improving patient satisfaction. Second, integrating nanoscale sensors and actuators enables more intuitive and responsive control of prosthetic limbs, advancing the field of neural rehabilitation and promoting user independence. Moreover, the potential for targeted drug delivery through nanomaterials offers pain relief and accelerates tissue healing, particularly valuable in postoperative recovery and wound management. The future prospects of hybrid nanomaterials in prosthetic devices are promising, with ongoing research exploring new functionalities, such as self-healing materials and neural interface technologies. Additionally, advancements in nanofabrication techniques and scalable manufacturing hold the potential to make hybrid nanomaterials more accessible and cost-effective. However, challenges such as long-term biocompatibility, regulatory approval, and ethical considerations in neural interface technologies require thorough evaluation. Overall, the potential advantages and future prospects of hybrid nanomaterials in prosthetic devices are indicative of a transformative era in the field of prosthetics, where technology converges with medicine to bring forth groundbreaking solutions that empower individuals with enhanced mobility and quality of life ( Antoniadou et al., 2011; Han et al., 2021; Li and Cheng, 2022; Ma and Baek, 2022; Tan et al., 2022).
CONCLUSION
The literature review on the applications of nanomaterials in prosthetic devices reveals several key findings. First, nanomaterials, including nanoparticles and nanocomposites, have been extensively explored in various types of prosthetics, such as bone prosthetics, skin prosthetics, and neural interfaces. These materials offer unique properties, such as improved biocompatibility, mechanical strength, and controlled drug delivery, which significantly enhance the performance and adaptability of prosthetic devices. Second, the integration of nanomaterials has led to the development of advanced nanocomposites that combine the principles of biomedicine and materials science. These hybrid nanomaterials exhibit tailored properties, such as lightweight yet durable structures, enabling prosthetic limbs to closely mimic natural limb behavior and function. Third, clinical testing and real-world performance of electric and myoelectric prosthetic limbs with embedded nanomaterials demonstrate remarkable advancements in prosthetic control and overall user experience. The seamless integration of nanoscale sensors and actuators allows for real-time feedback and adaptability, leading to more intuitive and responsive prosthetic control.
The overall impact of nanomaterials on the development and improvement of prosthetic devices is nothing short of revolutionary. Nanotechnology has ushered in a new era of prosthetics, where the once elusive goal of creating prosthetic devices that closely mimic natural limb behavior and adapt to users’ intentions becomes increasingly attainable. Nanomaterials have enabled significant improvements in prosthetic functionality, comfort, and longevity. Using nanocomposites, smart sensors, and drug delivery systems has addressed key challenges, such as mechanical strength, control, and biocompatibility, resulting in advanced prosthetic devices that enhance user independence, mobility, and overall quality of life. Additionally, the combination of biomedicine and materials science has played a pivotal role in unlocking the full potential of nanomaterials, facilitating their seamless integration into prosthetic devices and fostering interdisciplinary collaborations that drive further innovation in the field of prosthetics. While the literature review highlights significant advancements in using nanomaterials in prosthetic devices, several gaps in current research and potential areas for future investigation are identified. First, long-term biocompatibility studies are necessary to fully understand the effects of nanomaterials on the human body over extended periods. Continued research and thorough testing are essential to ensure the safety and efficacy of nanomaterial-based prosthetic devices in real-world scenarios. Second, standardization of manufacturing processes and quality control for nanocomposites and nanoscale components need attention to ensure the consistency and scalability of these materials in prosthetic devices. Third, ethical considerations surrounding nanoscale sensors and neural interface technologies require careful examination to address privacy, security, and user consent concerns. Moreover, efforts should be directed toward making nanomaterial-based prosthetic devices more accessible and affordable to a broader range of individuals with disabilities. Future investigation could also focus on integrating nanotechnology with other emerging technologies, such as artificial intelligence and robotics, to create even more sophisticated and adaptive prosthetic devices.
In conclusion, the literature review on the applications of nanomaterials in prosthetic devices reveals a transformative impact on the field of prosthetics. Nanomaterials have led to the development of advanced nanocomposites, smart sensors, and drug delivery systems, resulting in prosthetic devices with improved functionality, adaptability, and user experience. The combination of biomedicine and materials science has been instrumental in unlocking the full potential of nanomaterials, fostering interdisciplinary collaborations that drive further innovation in the field. While significant progress has been made, further research is needed to address gaps in long-term biocompatibility, standardization of manufacturing processes, ethical considerations, and accessibility. The future prospects for nanomaterial-based prosthetic devices hold immense promise, paving the way for a more inclusive and empowering future for individuals with disabilities.