Introduction
Heart failure (HF) is a growing public concern worldwide. Asian countries with large populations carry a much higher risk of HF compared to their Western counterpart. Most patients with HF in these countries are identified during admission for acute decompensated HF (ADHF), thus posing a substantial economic burden associated with high mortality during hospitalization, frequent readmissions and high mortality on follow-up. Data from ADHF registries in the past decade was predominantly due to HF with reduced ejection fraction (HFrEF). Over the past few years, HF with preserved ejection fraction (HFpEF) has been increasingly recognised as a major contributor to ADHF. Most available data are from Western countries, whereas limited regional and local data are available from the Asian countries.
A study from Asian HF registries has stressed the rising problem of multimorbidity in Asia [1]. Older, younger, ischemic and diabetic groups have vastly different presentation and outcomes from those in the Western world. Approximately 60% of the world’s population lives in Asia, where the population is expected to reach 5.2 billion by the year 2050. Lifestyle changes, and increased prevalence of diabetes mellitus (DM) and hypertension (HTN), have contributed to elevated ischemic heart disease (IHD) incidence and consequently HF burden. Poor socio-economic factors are a major concern in Asia. Data on HF are available for only a few Asian countries. Recent publications on HF in Asia have indicated overall poor outcomes, particularly in Southeast Asia [2].
In HF, decreased cardiac contractility activates the sympathetic and renin-angiotensin-aldosterone system (RAAS), thus leading to cardiac remodeling, and worsening of HF and the resultant consequences. The dilated heart is a substrate for arrhythmias by creating increased automaticity, triggered activity and re-entry circuits in areas with scar tissue. Fibrosis and regional hypertrophy predispose individuals to ventricular arrhythmias [3]. Action potential prolongation, a feature of failing hearts, occurs after alterations in K+ channel expression and calcium entry into cells in HF.
Sudden cardiac death (SCD) and ventricular arrhythmia in ADHF are associated with high mortality. Patients with HF have a rate of SCD six to nine times greater than that in the general population [4]. SCD accounts for 30–50% of deaths in individuals with HF [5]. Ventricular tachycardia/ventricular fibrillation (VT/VF) occurs in 20–80% of patients with HF [6]. In HFrEF, VT/VF are common, whereas bradyarrhythmias and pulseless electrical activity are less common. However, VT and VF have been reported to be uncommon in an investigator-reported analysis of HFmEF and HFpEF. In a pooled analysis of the PARAGON HF, TOPCAT, I-Preserve and CHARM-Preserved trials, only 1% of 13,609 patients had VT/VF (Incidence rate of 0.3/100 person-years). HFmEF patients had higher mortality than HFpEF and HFrEF [7].
The metabolic effects of acute HF are complex, and depend on its severity and associated comorbidities, such as diabetes and HTN. The failing heart is energy deficient, has diminished glucose, and depends on fatty acid oxidation [8]. Free fatty acids contribute to arrhythmias. Drug therapy, particularly angiotensin receptor-neprilysin inhibitor (ARNI) – sacubitirl/valsartan and sodium-glucose cotransporter-2 inhibitor (SGLT2i) in HF, addresses this metabolic derangement. Newer drugs are being developed to target this fatty acid metabolic pathway.
Guideline-directed medical therapy, particularly with beta blockers and ARNI, has substantially decreased the incidence of SCD. In the PARADIGM-HF trial, the primary outcome of cardiovascular mortality was decreased by 20% in the sacubitril-valsartan arm compared to the enalapril arm [9]. The various beneficial effects of ARNI in cardiac re-modelling, cardiac function, metabolic effects and decreased SCD have been well documented [10]. Thus, ARNI treatment has an important role in the therapy for HF [11].
This article analyzed data from Asian registries to understand these regions’ HF status, treatment patterns and outcomes. The merits and limitations of various registries are compared and discussed. Only limited data are available on chronic HF.
HF in Asian Countries
The Asian HF registry (Asian sudden cardiac death in heart failure) was a prospective observational registry study of Asian patients > 18 years of age with at least one episode of ADHF in the prior 6 months, conducted across 46 centers in China, Hong Kong, India, Indonesia, Japan, Korea, Malaysia, the Philippines, Singapore, Taiwan and Thailand between 2012 and 2016; both HFrEF and HFpEF were studied [2].
The primary outcome data of all-cause mortality were available in 5875 (90.7%) patients. The oldest patients were from Northeast Asian countries. Patients with HFrEF were at least 8 years younger than HF patients in other Asian countries. Women from Northeast Asia comprised 25.2% of the cohort, whereas 17.7% were from Southeast Asia. The youngest cohort members were from the Philippines. Southeast Asia HF patients had a higher prevalence of DM, HTN, chronic kidney disease (CKD) and coronary artery disease (CAD). IHD was the most common etiological factor. This cohort had the highest body mass of 26.9.
When GDMT for HF were analysed, the highest use of angiotensin-converting enzyme (ACE) inhibitors/angiotensin receptor blockers (ARB) and beta-blockers was from Southeast Asia (77.3% and 70.2%) respectively. ACE/ARB and beta-blockers were used in 81.8% and 78.9% of patients with HFrEF and HFpEF, respectively in southeast Asian countries. However, marked variation in use was observed among countries. Indonesia had the lowest beta-blocker use and relatively high use of ACE/ARB, whereas Japan had the highest use of beta-blockers.
The 1-year mortality in the Asian region was 9.6% (10.6% for HFrEF and 5.4% for HFpEF). Southeast Asia had the highest all-cause mortality (13.6%), as compared with 8.9% and 8.3% in Northeast Asia and South Asia, respectively. Despite having the youngest populations, Indonesia and the Philippines had the highest mortality rates, at 21.4% and 14.3%, respectively. The mortality rate was lowest in Japan, although the population with HF was older than that in other countries.
Patients from the lowest income group tended to be younger and to have the poorest outcomes. The Southeast Asian patients with ADHF had the highest number of comorbidities and higher mortality within 1 year. However, the 1-year mortality for HFrEF and HFpEF in the Asian cohort was higher (15% and 17%, respectively) than that in the SWEDE–HF (Swedish Heart Failure) registry [12], possibly because of a higher incidence of atrial fibrillation.
Analysis of patients with HFpEF in the Asian HF registry indicated that South Asian patients who had higher mortality rate had a high incidence of atrial fibrillation (AF), CAD and CKD, as well as a lower use of beta blockers and devices. Whether the lower mortality in Japan might be associated with higher use of beta blockers and devices warrants further study.
ADHF IN China
The prevalence of HF in China is approximately 1.3% in people above 35 years of age, and affects approximately 9 million people. Various registries have provided a picture of the current state of ADHF in China. In collaboration with global registries, earlier registries focused on chronic HF (INTER-CHF) [13] or were retrospective (CHINA PEACE) [14]. The prospective HF registries are as follows.
CHINA Heart Failure Registry
The China Heart Failure Registry-1 [15] included baseline data on HF, thus increasing understanding of various difficulties in diagnosing, treating, and following up patients with HF, as in many other HF registries in Asian countries. The recently reported China HF-II (2017–2020) study has indicated a changing scenario of HF in China [16]. The study was conducted in 113 hospitals and prospectively enrolled 34,938 patients. The data were compared with those in the Get With The Guidelines Heart Failure (GWTG-HF) registry [17]. The mean age was 67 years, and 60% were men. CAD accounted for 48.3%, valvular heart disease (VHD) accounted for 18.7%, and dilated cardiomyopathy (DCM) accounted for 16.3%. Hypertension was observed in 56.3% of patients, whereas diabetes was observed in only 36.3% of patients. The incidence of AF was high (17.6%). LVEF was found in 93.7% of patients (HFrEF, 40%; HFmEF, 21.8%; HFpEF, 38%). A total of 93% of patients had NT-pro-BNP measured.
The use of guideline-directed medical therapy (GDMT) significantly differed with respect to that in other countries: 78.7% received RAAS inhibitors; ARNI use was higher, at 36.5%; and 82.2% received beta-blockers. Mineraloreceptor antagonist (MRA) was used in 87.8% of patients, and ivabradine prescription was 8.3% at hospital discharge. The GDMT prescription rates in this registry were less than those in the GWTG-HF registry. However, only 3.9% and 14.6% of eligible patients received an internal cardioverter defibrillator (ICD) and cardiac resynchronization therapy (CRT). Notably, the in-hospital mortality rate decreased from 4% in the CHINA-HF-I registry to 2.8% in the CHINA HF registry-II. Despite the low in-hospital mortality, the hospital stay was long (9 days). ARNI and MRA use was higher in this registry than in the data from other Asian countries. NT-pro-BNP is a key feature for early diagnosis of HF. The remarkable improvement in the use of GDMT is commendable. Better reimbursement and low medication costs must have contributed to this improvement in GDMT prescription. The high GDMT prescription rates are one of the key features to learn, and they could probably be replicated elsewhere. However, a substantial limitation was the poor follow-up (only 27.5% of patients had at least one follow-up). This aspect is concerning, because HF therapy is life-long, and is associated with elevated long-term mortality and re-hospitalization rates.
Hero Registry
This prospective registry study was conducted in 73 provincial, municipal and county-level hospitals from November 2017 to November 2018. This study recruited 5620 patients [18]. The mean age was 72 years; 50% were women; and most were from rural areas. The percentage of comorbid conditions such as diabetes and HTN was low. VHD was the common aetiology, and the majority of ADHF patients had HFpEF. Only 57% received an echocardiogram. The use of diuretics was only 58%, a value much lower than the 90% reported worldwide. Only 52.2% and 61% received ACE/ARB and beta-blocker therapy, respectively. The hospital stay was prolonged but the in-hospital mortality rate was only 3.5%.
HF Registry from Southern China
A recent publication on the 5-year outcomes of HF in southern China has indicated that HFpEF is a growing problem [19]. In this study on 4880 patients from 2007 to 2014 with follow-up for 5 years, HFreEF affected approximately one-fourth of the study group. HFrEF had a twofold higher mortality than HFpEF. DM, HTN and CKD were observed in 28.99%, 39.65% and 36.65%, respectively. AF was observed in 8.84% of this group. ACE/ARB, beta blockers and MRA use were found in 55.87%, 76.06% and 68.65% of this HFrEF group.
HF in Korea
The prevalence of HF and the cost of HF therapy have been increasing in Korea. The first study on AHF enrolled 5625 patients with AHF in ten hospitals between 2011 and 2014 [20]. The mean age was 68.5 ± 14.5 years, which was comparable to the age in the Chinese registry. Approximately half the participants were men. A substantial percentage had LVEF analyzed, and 60% had HFrEF. Hypertension was observed in 62.2% of these patients, and DM was observed in 40%; 42.9% of the participants had IHD. The incidence of AF was as high as 28.5%. A total of 68.8% received RAAS inhibitors, 52% received betablockers, and 46.6% received MRAs at discharge [21]. The in-hospital mortality rate was 4.8%, and the mean length of hospital stay was 9 days, as observed in China. 14.6% of the ADHF patients had CKD. This is similar to the data from India. The 1-year mortality rate was 18%, a value comparable to that in other Asian countries. The prevalence of left bundle branch block (LBBB) and right bundle branch block (RBBB) was low. This probably reflects the lower use of cardiac resynchronisation therapy, which is indicated in HFrEF patients with LBBB.
A recent publication has indicated the increasing use of GDMT and better survival in patients with HF over the past two decades [21].
HF Registries in Japan
Only limited data are available from Japan. The JCARE-CARD study [22], published in 2011, has indicated that older patients with ADHF have poorer prognosis than younger patients. The more recent ATTEND [23] registry study was conducted in 53 regional hospitals from 2007 to 2011. The WET-HF [24] registry study was conducted on AHF in patients at a single center, and two hospitals were later added. The REALITY-AHF registry [25] collected data from 20 hospitals but examined the effects of early diuretic administration in AHF.
The data from a pooled analysis of 9075 patients have indicated a change in the treatment and outcomes of HF over the past two decades [26]. Patients with HF were older, but the length of hospital stay was shorter compared to the data from other Asian countries. However, the mortality and re-admission rates did not differ, despite the higher proportion of elderly HF patients. The mean age increased from 73 to 78 years, over 9 years. More than 55% of the enrolled patients were males. HFrEF decreased from 53% to 37%. Hypertension was very high (69%, 71% and 67%, respectively, in the ATTEND, WET-HF and REALITY-AHF). DM was observed in approximately one-third. The incidence of AF ranges from (36–49%) which was higher compared to the data from other Asian registries. The in-hospital mortality decreased from 6.4% to 5.1%. Unfortunately, data on GDMT are not available.
Indian Registries in Heart Failure
Trivandrum Heart Failure Registry
The Trivandrum Heart Failure Registry (THFR) was India’s first prospective HF registry with a 5-year follow-up. This hospital-based registry comprised patients admitted with HF in the city of Trivandrum and suburban area in Kerala, India, with populations of 957,000 and 166,549, respectively [27]. A total of 1205 patients with HF admitted between January 2013 and December 2013 to 16 hospitals in Trivandrum were enrolled. A total of 69% were men, the mean age was 61.2 years, 55% had HTN, 52% had diabetes, and CAD was the etiology in 72%. HFrEF was observed in 62%, HFpEF was observed in 20%, and HFmEF was observed in 18%. The in-hospital mortality rate was 8.4%, the 1-year mortality rate was 30.8%, and the 5-year unadjusted mortality rate was 59%. The 5-year mortality rate was 61.3% for HFrEF, 60.5% for HFmEF and 46.8% for HFpEF. The median survival time was 3.1 years. SCD occurred in 48%, and pump failure occurred in 48%. Baseline age, systolic blood pressure (SBP), functional class, serum creatinine and discharge GDMT were independent predictors of outcomes. The rate of hospitalization for HF was 49% in 5 years, and the mortality rate was higher in those with HF hospitalization (HFH) (69% in those with HFH vs 50% in those without HFH) [28]. One-quarter of patients received GDMT at discharge, and <2% received ICD implantation. The survival rate was higher in those with than without GDMT. The data demonstrated high mortality in ADHF patients treated in India. This reflects poor GDMT prescription at discharge.
Medanta HF Report
This retrospective observational study was conducted at Medanta Hospital, New Delhi, on the basis of the medical records of patients with HF admitted between 2014 and July 2017. A total of 5590 patients were included, of 83% of whom were men and 77.8% of whom had CAD. The mean age was 59.1 ± 11.8 years. A total of 59% had LVEF below 30%, and AF was found in 5%. The rate of all-cause mortality at 1 year was 17.6% [29]. Age, serum creatinine, use of loop diuretics and ivabradine were independent predictors of mortality.
CSI-Kerala Acute Heart Failure Registry
This prospective registry included patients with acute HF admitted to 50 different hospitals across Kerala, with adequate representation of public sector, private sector, teaching and non-teaching hospitals [30]. The participating centers included 19 teaching hospitals and nine governmental hospitals. A total of 7507 patients were enrolled, of whom 65.7% had HFrEF, 17.6% had HfmEF, and 14.9% had HfpEF. A total of 63% were men, and the mean age was 63.4 years in patients with HFrEF and 66 years in patients in the other two categories. A total of 61% had diabetes, and 53% had HTN. IHD was the primary etiology (65.5%), and 65% had de novo AHF. AF was present in 14%, CKD was present in 15%, and anemia was present in 15%. ARNI prescription was extremely low (1.8%). Only 1.64% received device therapy. Ivabradine use was observed in 15%. The rate of in-hospital mortality was 7% (HFrEF was associated with the highest mortality, at 7.7%, whereas HFpEF was associated with 5.5% mortality). A total of 40% of the deaths were arrhythmic and due to VT/VF. Overall, the 90-day mortality was 11.6% (HFrEF, 12.3%; HFmEF, 9.9%; HFpEF, 10.6%), and the 90-day rehospitalization rate was 11.41% (HFrEF, 12.08%; HFmEF, 10.64%; HFpEF, 9.37%). Age, creatinine, EF, SBP and GDMT use were predictors of mortality.
Indian College of Cardiology National Heart Failure (ICC-NHFR) Registry
This prospective observational registry enrolled consecutive patients with HF admitted to various hospitals across India from August 2018 to July 2019. A total of 5269 participants were enrolled; 67% were men, and the mean age was 61.9 years. De novo HF was observed in 33.59%, in contrast to the Kerala AHF registry, in which de novo HF was 63%. DM was observed in 51.53% of patients, and HTN was observed in 52.24%. IHD was identified in 75%. AF was observed in 8.78%. LVEF was <40% in 68.29%. The rate of in-hospital mortality was 6.98%, 30-day mortality was 12%, and 30-day rehospitalization was 8.33%. GDMT at discharge was 25%. Use of ivabradine was 13% at discharge, and use of ARNI was only 2.68%. BB, RAAS and MRA were prescribed in 68%, 42.67% and 45.97%, respectively, at discharge. Age, creatinine and LVEF <40% were independent predictors of 30-day mortality [31].
ICMR-NHFR Registry
NHFR is a facility-based registry of patients with ADHF admitted to 53 hospitals in 21 states and four union territories in India between July 2019 and July 2020. A total of 10,851 patients were enrolled in this registry [32]; 69% were men, and the mean age was 59.9 years. Almost 75% had de novo HF. HFrEF was observed in 65.2%; 72% had ischemic etiology; 58.9% had HTN; 42.3% had diabetes; 8.5% had CKD; and 9.5% had atrial arrhythmias. A total of 47.5% of patients with HFrEF received GDMT. ARNI use was 4.8%. This is an increasing trend in ARNI prescription rates in ADHF. The rate of in-hospital mortality was 7.55% for HFrEF and 5.1% for HFmEF. Hospital readmission at 90 days was 8.4%. Overall, the 90-day mortality was 14.2%. HFpEF had 23% lower mortality than HFrEF at 90 days. Educational status, pedal edema, hemoglobin, mitral regurgitation, serum sodium levels and AF at baseline predicted the 90-day mortality. The 90-day mortality was highest in those with the lowest educational status. GDMT was associated with improved survival in patients with HFrEF and HFpEF.
THAI ADHERE Registry
This multi-center prospective observational registry enrolled 1612 hospitalized patients with a discharge diagnosis of HF at 18 centers in Thailand between March 2006 and November 2007. The median age was 67 years, and 23% of the cohort was older than 75 years. The numbers of men and women were nearly equal, in contrast to most other Asian registries. A total of 66.5% had previous HF; 47.3% had diabetes; 64.8% had HTN; 19.8% had CKD; and 24% had AF. One in five required mechanical ventilation. CAD was the most common etiology (44.7%). The rate of in-hospital mortality was 5.5%. One-fifth died of worsening HF, 9% died of arrhythmias, 13.3% died of ischemia, and one-third died of noncardiac causes. SBP <90 mmHg, CKD, NYHA class IV and history of stroke were independent predictors of mortality. Only 60% had EF assessed, and 43.6% had LVEF <40%. A 10-year follow-up study based on the same cohort has found a 10-year mortality of 73.3%. The mortality at 1 month, 6 months, 1 year, 5 years and 10 years was 8.1%, 21.1%, 28%, 58.2% and 73.3%, respectively [33]. The 5-year mortality was similar to that in the THFR.
THAI-AHF Registry
The THAI-AHF Registry enrolled 759 patients between July 2017 and June 2019. The mean age was 68.9 ± 15 years, and the male/female distribution was equal. The in-hospital and 1-year mortality rates were 5.8% and 21.5%, respectively. This is the most recent registry from Thailand [34].
TSOC-HFrEF Registry
This prospective multicenter registry enrolled 1509 patients admitted with HF to 21 Taiwanese centers from May 2013 to October 2014. The mean age was 64 years, and 72% were men. One-third had HTN, 43.65% had DM, and 31.6% had CKD. AF was documented in 26.7%, and 8.8% had LBBB. 27.4% had eGFR <30 mL/min/sq m. Hyponatremia was detected in one-fifth, and 3.6% received device implantation during hospitalization (1% ICD; 0.8% CRT-P; 0.4% CRTD). The rate of in-hospital mortality was 2.4%. Low SBP, CKD, ICD/CRT implantation and concomitant COPD were independent predictors of mortality [35].
Malaysian HF Registry
This 3-year prospective observational registry comprises acute HF admissions at 18 sites in western and eastern Malaysia. A total of 2717 patients were enrolled between August 2019 and December 2020. The median LVEF was 34%. HFrEF was observed in 64.6%, HFpEF was observed in 21.6%, and HFmEF was observed in 11.4%. The mean age was 60+17 years, and 66.8% were men. A total of 71% had HTN, 60% had diabetes, and 31% had CKD. Moreover, 10% had anemia, 16% had AF, and 3% had LBBB. At discharge, 94% had at least one HF medication. Triple therapy of beta-blockers, RAAS inhibitors, and MRA was prescribed to one-third (28.6%) of ADHF patients at discharge. The rate of in-hospital mortality was 2.9%. The cause of death was worsening HF in nearly 50% and cardiac arrest in approximately one-fifth (18%) [36].
The Philippines HF Registry
This registry is part of the OPTIMISE-HF registry started in 2014 [37]. The HF registry enrolled 636 patients between 2014 and 2018. The mean age was 56.7 ± 15.2 years. 60.1% of ADHF patients were males. Hypertension was observed in 35.7%, DM was observed in 24.4%, and CKD was observed in 8.3%. IHD contributed to 50% of the cases. RHD was observed in 7.5%. Only 54.9% received ACE/ARB. Beta-blockers were used in 47.5% of the group, and MRA was used in 26.5%. The rate of in-hospital mortality was 3.9% [38].
Lessons Learned
Among registries, China HF II enrolled the most patients, most of whom underwent biomarker testing. The GDMT prescription rates in China were higher compared to the data from other Asian registries. The mean length of hospital stay, 9 days, was higher than in the data from other Asian HF registries. The percentage of patients discharged early for treatment at home, on the basis of patient preferences was a major hurdle in obtaining follow-up data. China HF II registry showed the lowest ADHF mortality rate in Asia. Suggestions to improve follow-up care are required. The TSOC-HFrEF registry from Taiwan reported the lowest mortality, at 2.4%, but has the drawback of a relatively small number of enrolled patients.
India’s THFR was one of the earliest ADHF registries. Despite being conducted in a small district, the study reported valuable findings regarding high mortality and poor adherence to GDMT. The report clearly demonstrated the effects of GDMT and mortality, and led to two large national registries and one state registry, which were well conducted and reported corroborating findings of high in-hospital mortality, at 7%, and GDMT prescription to 25% of patients at discharge. The findings have led to many quality improvement measures. Moreover, the 5-year follow-up data have provided valuable insights for planning policy decisions in HF care.
The Korean registry is commendable for its long-term follow-up and large sample size. The follow-up mortality data have been published, thus aiding in formulation of better strategies to improve care. The Japanese registry data are insufficient to draw any definitive conclusions. However, the trends over the past few years in Japan have indicated clear changes: better GDMT adherence, specifically beta-blockers and device usage, and a higher percentage of elderly patients in ADHF. The Thailand cohort was part of the global ADHERE registry. Being part of the global registry, the enrolments were few. The in-hospital mortality of ADHF was comparable to the data from other Asian countries. The major concern is the higher mortality and rehospitalization on follow-up. The strengths and limitations of the various registries are outlined in Table 1, to aid in planning appropriate regional strategies.
Overview of Demographics, Etiology and Outcomes of HF in Asia.
| - | Total No | Age | Sex (%) | DM | HTN | CKD | AF | IHD | LVEF <40% | >40% | NT-PRO BNP | BB | ACE/ARB/ARNI | MRA | Mortality in hospital | 30 Day | 90 Day | 1 Year | Rehospitalisation 30 days | Rehospitalisation 90 days | Rehospitalisation 1 year | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | W | |||||||||||||||||||||
| Asian HF | 6480 | 61.6 ± 13.3 | 73 | 27 | 40.98 | 26.49 | 35.67 | 19.7 | 45.9 | 81 | 19 | - | 72.2 | 70.4 | 49.7 | - | - | - | 9.6 | - | - | |
| China HF I | 13687 | 65 ± 15 | 40.9 | 59.1 | 21 | 50.9 | - | 24.4 | 49.6 | 46.9 | 53.1 | - | 25.6 | 27.0 | - | 4.1 | - | - | - | - | - | - |
| China HF II | 34 938 | 67 ± 14 | 60.8 | 39.2 | 31.5 | 56.3 | - | 17.6 | 48.3 | 38 | 62 | 93 | 82.2 | 78.7 | 87.8 | 2.8 | - | - | - | - | - | - |
| TSOC-HFrEF registry | 1509 | 64.0 ± 15.8 | 72.4 | 27.6 | 43.6 | 34.5 | 31.5 | 26.0 | - | - | - | - | 59.6 | 62.1 | 49 | 2.4 | - | - | 15.9 | - | - | 38.5 |
| Korea HF | 5625 | 68.5 ± 14.5 | 53.2 | 46.8 | 40 | 62.2 | 14.3 | 28.5 | 42.9 | 60.5 | - | 93.1 | 49.9 | 65.9 | 44.9 | 4.8 | 3.3 | 8.4 | 18.2 | 7.0 | 13.5 | 23.1 |
| Trivandrum Heart Failure Registry (THFR) | 1205 | 61.2 ± 13.7 | 69 | 31 | 52 | 55 | 54.6 | 72 | 62 | 20 | - | 58 | 48 | 46 | 8.4 | - | - | 30.8 | - | - | - | |
| Medanta HF | 5590 | 59.1 ± 11.8 | 83 | 17 | 18.1 | 49.2 | 48.9 | 5.0 | - | 59.1 | - | - | 81.8 | 65.8 | - | - | - | - | 17.6 | - | - | - |
| CSI-Kerala Acute Heart Failure Registry | 7507 | 64.3 ± 12.9 | 63 | 37 | 61.5 | 53 | 14.8 | 14 | - | 67.5 | 14.9 | - | - | 74.9/53.6/2.9 | - | 7 | - | 11.6 | - | - | 10 | - |
| Indian College of Cardiology National Heart Failure (ICC-NHFR) registry | 5269 | 61.90 ± 13.85 | 67.09 | 32.91 | 51.53 | 52.27 | 14.81 | 8.78 | 75.44 | 68.29 | 31.71 | 29 | 67.18 | 41.18 | 49.08 | 6.98 | 5.37 | - | 20.82 | 7.98 | - | - |
| ICMR-NHFR registry | 10851 | 59.9 | 69 | 31 | 42.3 | 48.9 | 8.5 | 9.5 | 72 | 65.2 | 12.7 | - | - | - | - | 6.7 | - | 14.2 | - | - | 8.4 | - |
| THAI ADHERE registry | 2041 | 64 ± 14 | 49.6 | 50.4 | 47.0 | 65.0 | 19.0 | 24.0 | - | 43.6 | - | - | 25.2 | 35.3/12.4 | - | 5.4 | - | - | - | - | - | - |
| Malaysian HF registry | 2717 | 60.2 ± 13.6 | 66.8 | 33.2 | 59.8 | 71.5 | 30.9 | 16.1 | 55.9 | 64.6 | 21.6 | 81.5 | 81.1 | 37.6/8.4/15.7 | 43.6 | 2.9 | - | - | - | - | - | - |
| Japanese Cardiac Registry of Heart Failure in Cardiology | 2676 | - | 69 | - | - | - | - | - | 32 | 58 | 42 | - | - | - | - | - | - | - | - | - | - | - |
| Philippine HF registry | 636 | 56.7 ± 15.2 | 60.1 | 39.9 | 24.4 | 39.3 | 8.3 | - | 50 | 100 | - | - | 47.5 | 54.9 | 26.5 | 3.9 | - | - | - | - | - | - |
| HERO Registry | 5620 | 72 | - | 50 | - | - | - | - | - | - | - | - | - | 52.2 | 61 | 3.5 | - | - | - | - | - | - |
| HF registry from Southern China | 4880 | - | - | - | 28.99 | 39.65 | 36.65 | 8.84 | - | - | - | - | 76.06 | 55.87 | 68.65 | - | - | - | - | - | - | - |
| HF registries in Japan | 9075 | 71.6-77.0 | - | - | - | - | - | - | - | - | - | - | - | - | - | 4.7–7.5 | - | - | - | - | - | - |
| THAI-AHF Registry | 759 | 68.9 ± 15 | 49.8 | 50.2 | 49.8 | 67.1 | 25.2 | 35.4 | 40.7 | 55.7 | 44.3 | 10,711.2 ± 10,731 | 53.4 | 36.7 | 14 | 5.8 | 3.1 | - | 21.5 | 24.2 | - | 63.9 |
Asian HF, Asian Heart Failure; CHINA HF I, CHINA Heart Failure Registry I; CHINA HF II, CHINA Heart Failure Registry II; Korea HF, Korea Heart Failure; THFR, Trivandrum Heart Failure Registry; Medanta HF, Medanta Heart Failure; CSI-KAHFR, CSI-Kerala Acute Heart Failure Registry; ICC-NHFR, Indian College of Cardiology-National Heart Failure Registry; ICMR-NHFR, Indian Council of Medical Research Registry-National Heart Failure Registry; THAI ADHERE, THAI Acute Decompensated Heart Failure Registry; TSOC-HFrEF, Taiwan Society of Cardiology-HFrEF Registry; Malaysian HF, Malaysian Heart Failure Registry; Philippines HF, Philippines Heart Failure Registry; HERO, Heart Failure Registry of Patient Outcomes; HF Registries of Japan, Heart Failure Registries in Japan; THAI AHF-THAI Acute Heart Failure Registry.
The available data clearly indicate that HF affects the Asian population at younger ages than its Western counterparts (Table 2). A male predominance is clear; however, whether this finding is associated with women not receiving the necessary attention and care is a matter of debate. The significant comorbidities are DM in Southeast Asia and HTN in Southern Asia and Southeast Asia. CKD is increasing and is a significant factor to be considered in HF treatment. IHD is the predominant etiology, ranging from 48% to 75% across Asia. An abnormal ECG is observed in approximately 90% of patients with HF in India;31 this essential aspect must be considered in planning treatment for patients with HF. Echocardiography usage requires greater emphasis in China and Thailand. In Asian populations, in contrast to the Western population, HFrEF is the primary entity and warrants greater attention, given the presentation at younger ages and the many effective therapies available.
Analysis of Various Asian Registries.
| Country | Merits | Limitations |
|---|---|---|
| India | Large numbers, many national registries studied, predominant HFrEF, many comorbidities identified | High in-hospital mortality, poor GDMT, low ARNI and device use |
| China | Large number studied, high use of NT pro-BNP, low in-hospital mortality | A smaller number of HFrEF enrolment and a higher HFpEF percentage |
| Japan | Small countries with high use of BB and devices | Limited data resources, older individuals, high AF |
| Thailand | Small country with good follow-up data | Small numbers and few centers |
| Philippines | Only HFrEF studied, low in-hospital mortality | Small number of patients enrolled, not representative |
| Korea | Excellent data and follow-up, low in-hospital mortality, high biomarker use | High AF, CKD prevalence |
| Malaysia | Low in-hospital mortality | Small numbers, poor follow-up |
As a diagnostic measure, NTpro-BNP is relatively less used in the Indian subcontinent (29%) [31] than in China, where the utilization rate exceeds 90% [19]. This crucial area requires greater education among physicians. Use of this measure would lead to earlier diagnosis and require less expensive point-of-care test availability. NTpro-BNP is likely to be used similarly to troponin in routine care.
A highly relevant finding was the use of GDMT in the Asian subcontinent (Table 2). Beta-blocker use is higher in Japan, China and Korea than in the Indian subcontinent. The use of RAAS inhibitors is slowly increasing but remains low in Southeast Asia. ARNI is very seldom used in Asia, except in China. MRA use is improving. However, GDMT prescription rates are far behind the contemporary data from the Western world (as observed in the EMPEROR [39] and DAPA HF trials) [40]. The use of SGLT2 inhibitors is improving, but most registries have not captured this use, given that the guideline recommendations were only recently released [12]. The primary concern is adherence to therapy.
The in-hospital mortality varies from 2.8% to 8.4% in various Asian ADHF registries (Figure 1). China has successfully decreased mortality over the years, as indicated in the China HF II registry data. Japan, Taiwan and Korea have impressively decreased mortality. India has a relatively higher mortality, close to 7%. However, the length of hospital stay is 9 days in China compared with 5 days in India. Long-term mortality data are available in only several countries (Figure 2). This crucial area must be addressed, because HF is a disease requiring long-term follow-up and management.
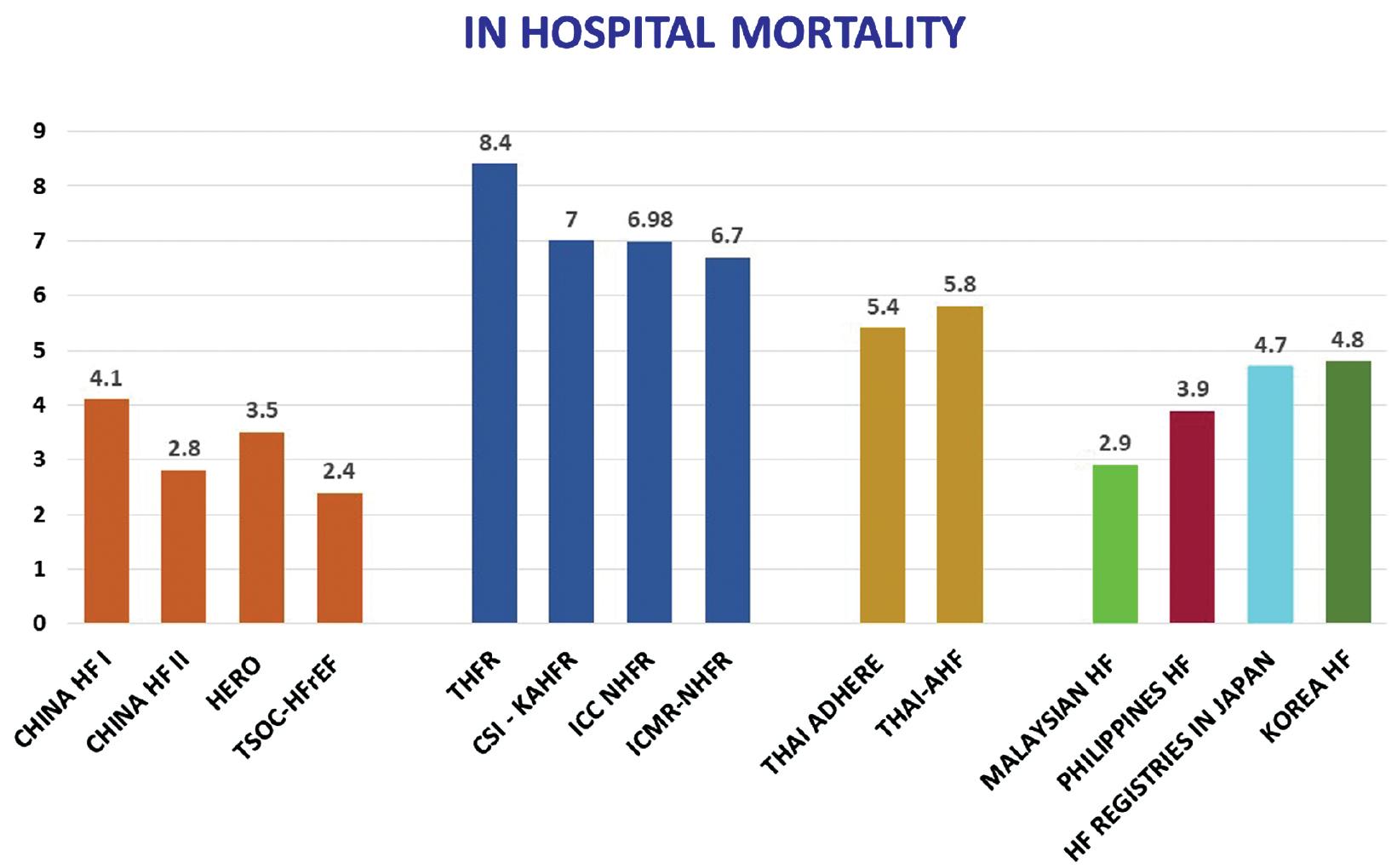
ADHF In-hospital Mortality in Asia.
CHINA HF I, CHINA Heart Failure Registry I; CHINA HF II, CHINA Heart Failure Registry II; HERO, Heart Failure Registry of Patient Outcomes; THFR, Trivandrum Heart Failure Registry; CSI-KAHFR, CSI-Kerala Acute Heart Failure Registry; ICC-NHFR, Indian College of Cardiology-National Heart Failure Registry; ICMR-NHFR, Indian Council of Medical Research Registry-National Heart Failure Registry; THAI ADHERE, THAI Acute Decompensated Heart Failure Registry; THAI AHF, THAI Acute Heart Failure Registry; TSOC-HFrEF, Taiwan Society of Cardiology-HFrEF Registry; MALAYSIAN HF, MALAYSIAN Heart Failure Registry; PHILIPPINES HF, PHILIPPINES Heart Failure Registry; HF REGISTRIES OF JAPAN, Heart Failure Registries in JAPAN; Korea HF, Korea Heart Failure.
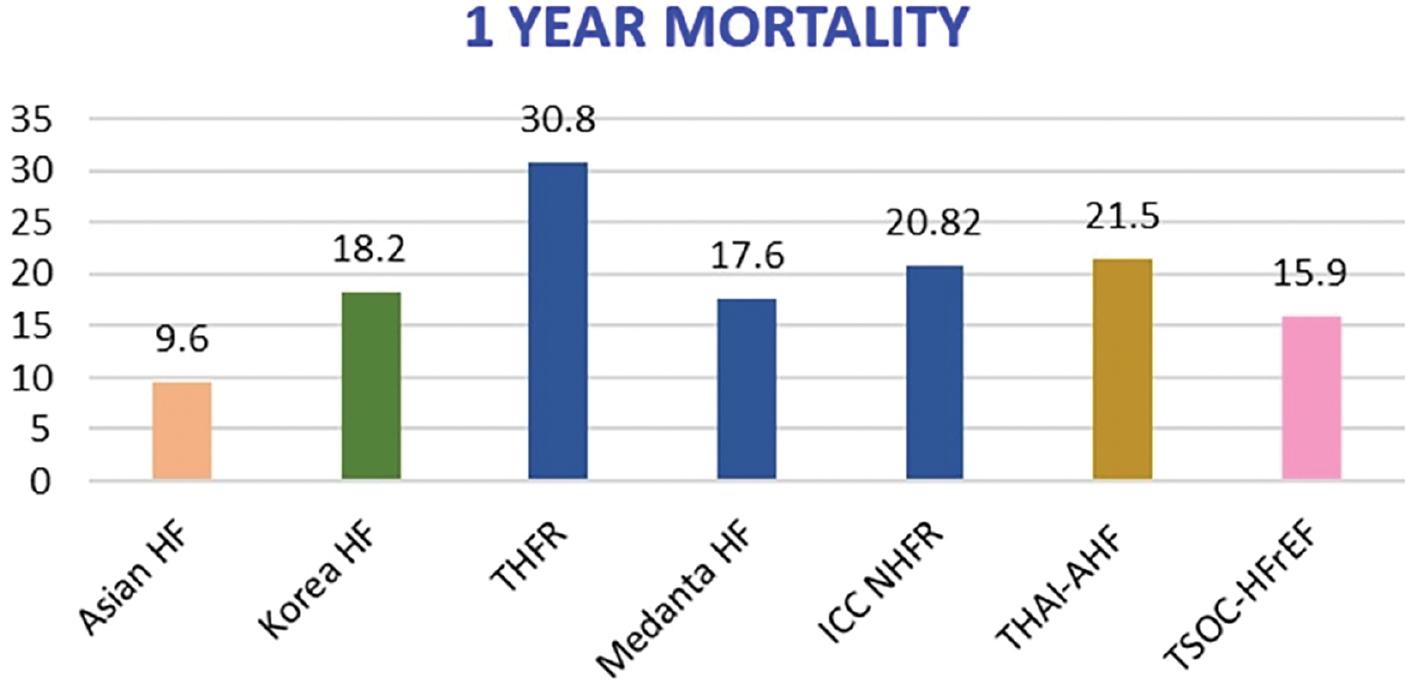
ADHF 1 Year Mortality in Asia.
Asian HF, Asian Heart Failure; Korea HF, Korea Heart Failure; THFR, Trivandrum Heart Failure Registry; Medanta HF, Medanta Heart Failure; ICC-NHFR, Indian College of Cardiology-National Heart Failure Registry; THAI ADHERE, THAI Acute Decompensated Heart Failure Registry; TSOC-HFrEF, Taiwan Society of Cardiology-HFrEF Registry.
The various ADHF registries in India have indicated a mortality of 18–20% in 1 year. The follow up data in China HF registries are not available. This needs to be addressed. In India, obtaining follow-up data beyond 1 year is challenging. All HF patients are enrolled in the Swedish and Danish registries. A similar process needs to be followed in every country. This will help in the follow-up of HF patients who need lifelong therapy. Device therapy use is very poor, and the priority is adherence to medical treatment.
Recent data on HFpEF have emerged from Southeast Asia. In a recent study from Malaysia, 15% of patients with ADHF from 2009 to 2018 [36] had HFpEF. These patients were relatively older and had HTN, diabetes, and AF. Although they were relatively stable and had better outcomes during admission, their 1-year mortality was higher than observed in the Asian HF cohort (37.9% versus 12.1–23.6%).
Critical needs include early diagnosis, GDMT implementation, and treatment adherence. Moreover, physician education, public education and the involvement of policymakers are necessary to ensure the cost-effective availability of ECG, biomarkers and echocardiography. Many state governments are ensuring that GDMT (Ace inhibitors, Beta-blockers, MRA and SGLT2 inhibitors) is free of cost at the primary care level. Generic medication availability has decreased treatment costs. Adherence to therapy can improve only if HF care teams are established, clear protocols are defined, available resources are used, and HF clinics are opened.
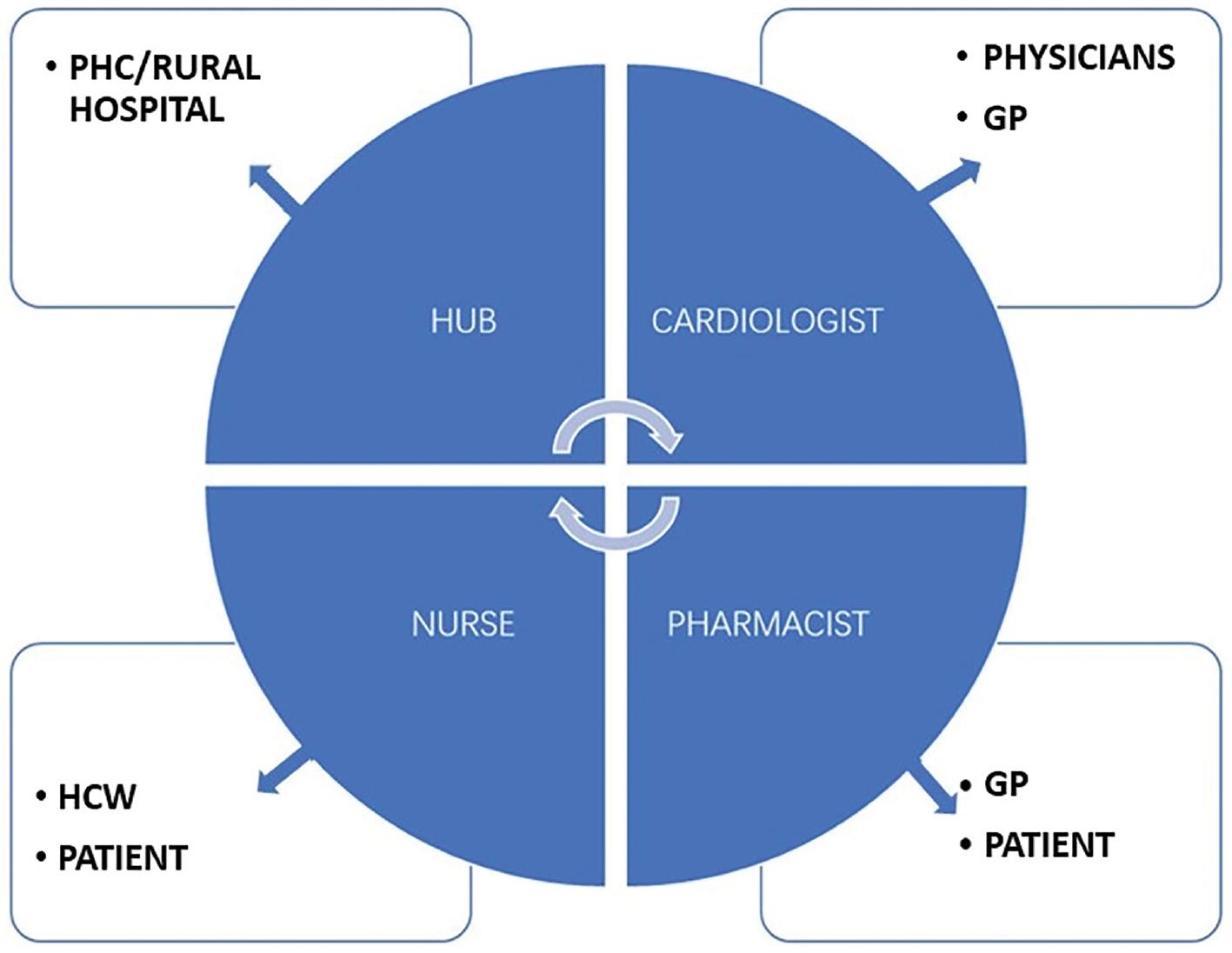
The roles of HF clinics, nurses, pharmacists, specialists and physicians are essential and remain major priorities [41]. Addressing these priorities would lead to better follow-up by ensuring that patients are discharged with a medication checklist, and given diet and fluid intake instructions. A point of contact with HF-trained nurses aids in follow-up and has been found to be effective in a study from South India [42]. The importance of ongoing registries with software for uploading data will be a crucial step in helping maintain standards of care and follow-up.
The accessibility of health care, differences in infrastructure, late presentation, non-availability and non-adherence to medication, lack of organized HF clinics and use of different care systems among countries are all possible reasons for the observed regional differences. Every region requires a different approach to address gaps in care [43]. The Taiwan heart registry has clearly indicated that continuing education for physicians and patients can improve HF care. Thus, registries will have crucial roles in the future. Running HF registries helps in understanding the current HF scenario, ensuring documentation, and planning future initiatives to identify gaps to improve HF care.
Our vision is to develop a standard of care in developing countries, as shown in Figure 3. Close coordination among team members is vital, and periodic assessment of quality standards and auditing are crucial. The presentation of data at regional, state, national and international forums, as well as discussions among experts, would help improve care systems. The future holds promise of collaboration among many partners in HF care.
Conclusion
Asia is a heterogeneous continent with a substantial population. Data on HF from Asia are limited. Low socio-economic status and multiple co-morbidities make provision of care challenging. Younger patients are increasingly affected, and IHD is the major aetiology for ADHF. Hypertension is a growing problem, as is CKD. Diagnosis is primarily clinical, and use of biomarkers and echocardiography must be further improved. GDMT utilization is poor, and adherence to therapy is even lower. Depending on the region, new innovative strategies must be planned to improve care. Given the multiple co-morbidities, a team approach and specific focus on opening HF clinics are recommended. The registries have highlighted the current scenarios and should serve as a basis for implementing measures to improve HF care. Clear documentation and follow-up using digital technology are attractive options for better follow-up of this group of patients.